Yesterday I presented the quick cheap ways to make the mental health service better. Today I present two, more expensive ones.
- Simplify the mental health system
- Train psychiatrists, therapists, social workers and other people involved in mental health services to recognise undiagnosed neurological conditions.
- Simplify the mental health system
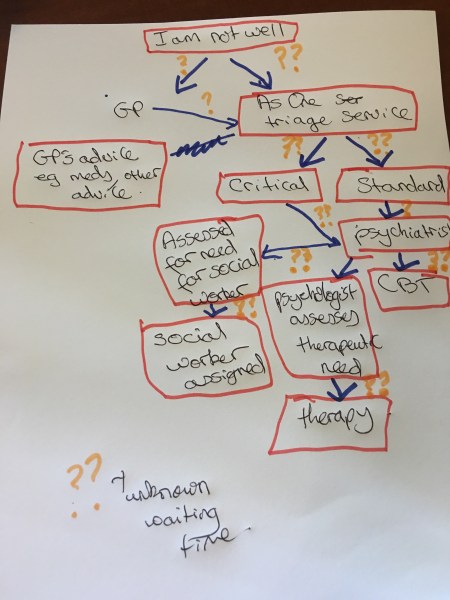
As I explained yesterday under the current system in the NHS in Hertfordshire, and I suspect elsewhere, a patient with a chronic mental health problem has to see many (in Hertfordshire it can be up to six) mental health professionals before receiving therapy – and patients have to explain their personal story, who they, perhaps, have not explained to anyone else, to each new person. If you are a happy person this would make your weary. If you’re a depressed person just dealing with the system could literally send you over the edge. However, the private system in the UK doesn’t work that and I think the NHS should copy the private system. In my experience if you want to go private this is what happens: – You go to your GP and you tell them that you are depressed. If s/he thinks that you need more specialist help she will write a referral letter. You phone up your insurance company and if you have funding in a week’s time you can be sitting in a psychiatrist’s office (obviously if you haven’t got funding your stuffed, but that’s a different matter). The psychiatrist is the first, and perhaps only, person that will take a detailed account of your history and s/he decides the best course of action to take eg Do you have a particular diagnosis that needs medication eg schizophrenia, bipolar, an anxiety disorder, Do you need therapy?, What sort of therapy?, Is there a therapist who would be a good ‘fit’ to your particular personality and that convenient for you to get to? How much therapy is required? Is the situation desperate – should this person go to hospital? If say the psychiatrist prescribed you ten therapy sessions s\he might see you after that period to assess whether you need more therapy/ medication. It’s just simple – you see one GP, one psychiatrist and one therapist and ideally you should see the same people on an ongoing basis. Of course, it doesn’t mean that people do not suffer, or die. Conditions are hard to treat, and wrong diagnoses are made (see point two below). But it does mean that the system is easier to understand and there is less chance of people falling through the gaps.
- Train mental health professionals to recognise undiagnosed neurological conditions
Everyone knows the a story of the boy, who is not doing that well at school, whose behaviour goes off the rails, who has a single mother with a full-time job and two other kids from other relationships. Although the mother loves her son very much, she has a below average literacy level, and she never does homework with him. In manhood, this boy can go one of two ways – either to prison or on the bright side – have low paid jobs and on and off anti-depressants for the rest of his life (there is of course a the third possibility – that he find a passion like music, which dramatically increases his self-esteem, and although difficult, he works hard to improve his literacy and ends up having a career in music, a loving family and very much enjoys life). In either of the first two examples the man goes to see a therapist and at the back of her mind the therapist is asking herself, ‘Why is this man depressed? What made him this way? I can see that he had a difficult childhood but I think I am missing something’. The man, of course, has undiagnosed dyslexia. The reason that the therapist is asking herself this question is because she has absolutely no training in recognising dyslexia or for that matter any other neurological condition like ADHD, autistic spectrum disorder (ASD), dyspraxia, and indeed epilepsy. She is trained primarily to listen and to understand personality traits and how people behave in relationships. And as a mental health professional she is not alone in not being able to recognise these conditions – many psychiatrists, in my experience, are not able to recognise them or think that these conditions occur only in children. Therefore, although the therapist might be able to treat emotional issues that her patient might have, from other experiences in life, she will never be able to address the underlying cause of her low self-esteem because dyslexia isn’t something she is trained to treat.
Rabbi Tatz argued, (get reference) that depression is caused by a lack of achieving your potential. That is why I believe I got depressed – I knew I was different from other people – but I didn’t know how and I couldn’t explain it to anyone because I didn’t his is why I believe I got depressed. And I am not alone – people with ADHD, ASD, epilepsy etc are just much more likely to get depressed[1] than other people. But if as I did, they go to a therapist, to treat this illness, they are unable to because it hasn’t been diagnosed and they don’t have the skills required to recognise it – let alone treat it (of course the patient could have of issues that a therapist could help with but there will always be a part of the patient that goes untreated),
Thus I believe that all mental health professionals, including therapists, psychiatrists, social workers and even GPs should be trained to spot these neurological conditions so they can refer patients who they suspect have one onto the appropriate professional and receive the appropriate care.
So that’s it Sharon’s mental health manifesto – part two. It’s expensive – but could be cheap in the long run.
PS Sorry if this blog sounds a bit antsy, but for those of you that don’t know I have been stuck in a big brother room for four days with 27 electrodes on my head being videoed monitored so the docs can see if I am having seizures. Tomorrow I get out – freedom!
[1] https://www.epilepsy.org.uk/info/depression https://adaa.org/understanding-anxiety/related-illnesses/other-related-conditions/adult-adhd# http://www.autism.org.uk/about/health/mental-health.aspx